Web-site restrictions
ACAT will be moving to a new web site on Thursday, 10th April.
In preparation, from Friday, 4th April this old web site will not let members renew their membership, and any other changes members make, e.g. their personal details, will get ‘lost in the move’.
Urgent membership renewals should instead be done by contacting Alison Marfell.
Draft States of Mind Inventory
Hubbuck, J., 2008. Draft States of Mind Inventory. Reformulation, Winter, pp.15-25.
Preliminary Tests in Individual and Group CAT Therapy at the Manor Clinic, Southampton
Introduction
In my previous article in ‘Reformulation’ (Hubbuck, 2008), I indicated that I was trying to devise a States of Mind Inventory (SMI), as a possible scored clinical measure, pre- and post-therapy. This idea followed on from my work with Dr Anthony Ryle on the States Description Procedure (SDP) and the later States Characterisation Procedure (SCP). (Ryle, 2007b). This article seeks to do the following: (a) briefly, to describe the origins of this draft SMI format; (b) to outline the SMI preliminary test results, and plans for further research testing of it, probably in 2009; (c) also very briefly, to indicate its integral role in CAT group therapy at the Manor Clinic; and (d) to explain the theory behind the use of this SMI in my individual and group practice.
In his ‘Afterword’ to my previous article Ryle encouraged CAT practitioners in general to use the SCP method. Maybe some other colleagues are now starting to use the SCP, but they have not yet used it enough to make their own judgements on its value to them or their patients. The integrated use of the SCP and the SMI could be a key topic for the 2010 ACAT Annual Conference, given the need for further tests of both during 2009.
Origins of the SMI
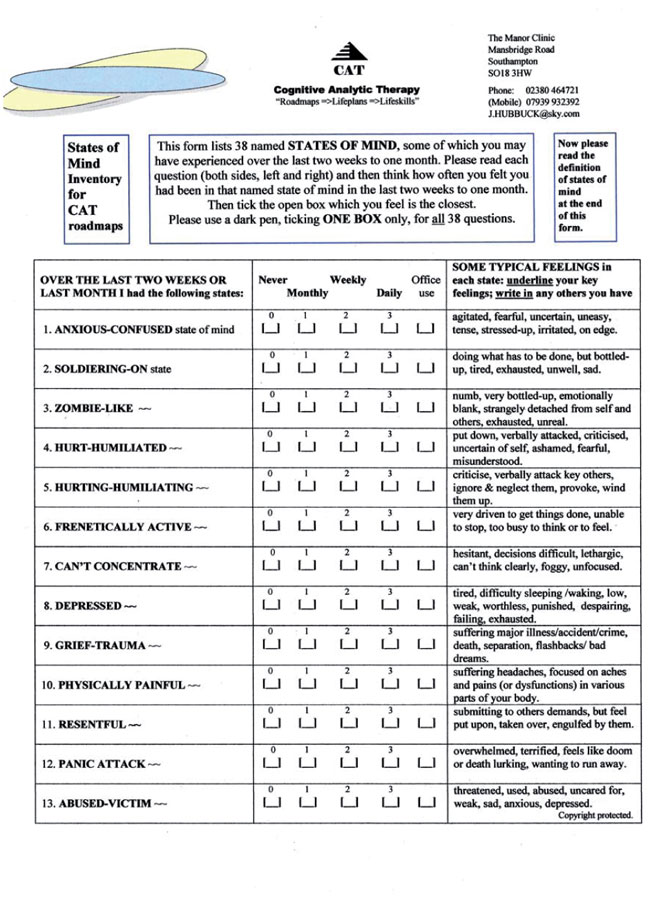
The draft SMI, containing 38 named states, is reproduced in Appendix 1. As stated above it originated from my earlier SDP/ SCP work. 29 out of 32 ‘borderline personality disorder’ (BPD) patients (90.6%) who had filled in the SDP questionnaires had said that this method had been either of value, or of considerable value, to their therapy. BPD patients felt that they had gained from the more precise naming of their painful states of mind, and from describing the frequency, duration, intensity and range of their subjective feelings when in these named states. Obviously, my patients had never really looked at their painful states in such self-analytical detail before. I hope that those colleagues interested in starting to use the SCP method will consult the pro-forma SCP reports, included at the end of my last article. These will probably help you to see more clearly how memory and meaning, affect and attitude, action and dialogic interaction, are wrapped up in named states of mind. Subjective states, combined with associated reciprocal role procedures (RRPs), can probably lay claim to being a central organising function of the human mind (brain) and personality. (Ryle, 1997; and Siegel, 1999).
The SCP aims to identify, in more detail, a limited number of key states of mind, within core RRPs, which are thought to be important in the aetiology of personality disorders. The SCP then helps this process of detailed state recognition to be transformed into a reciprocal understanding of core RRPs, which are often enacted by the patient towards the therapist, during therapy. The Clinical Outcomes in Routine Evaluation (CORE System Group, 2006) questionnaire is a market leader for clinical scoring of poor social-psychological functioning. And the CORE refers to mood states, but tends not to give these states clear-cut names. Also it is not precise in measuring intensity, frequency and duration of mood states. So this gave me the idea that CAT also doesn’t need to be inhibited by limited precision on such intensity, frequency, duration indices, in devising the draft SMI. My aim is to let you make your own judgements on this new SMI, without labouring the step by step, detailed thinking going into its development.
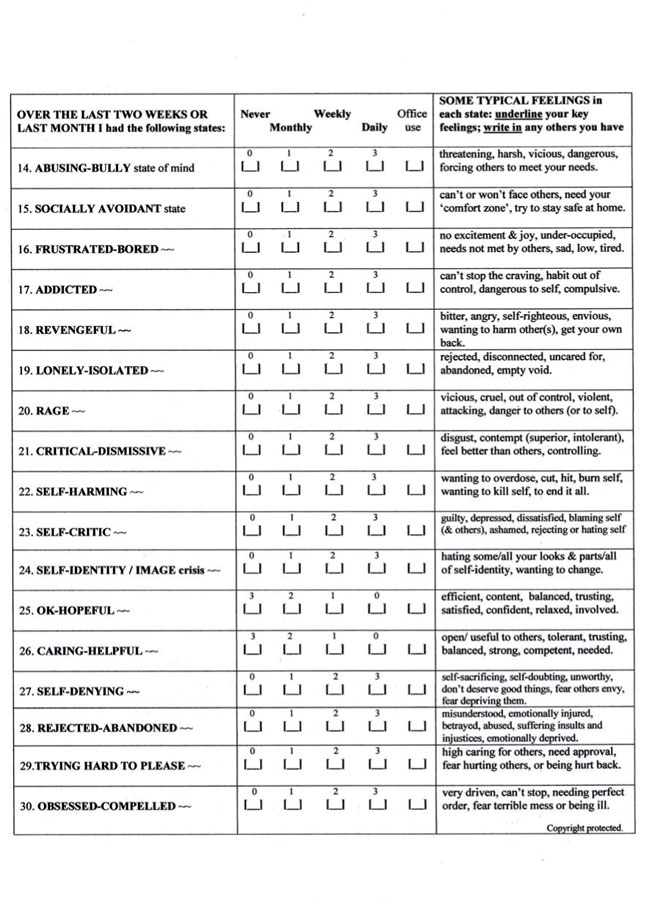
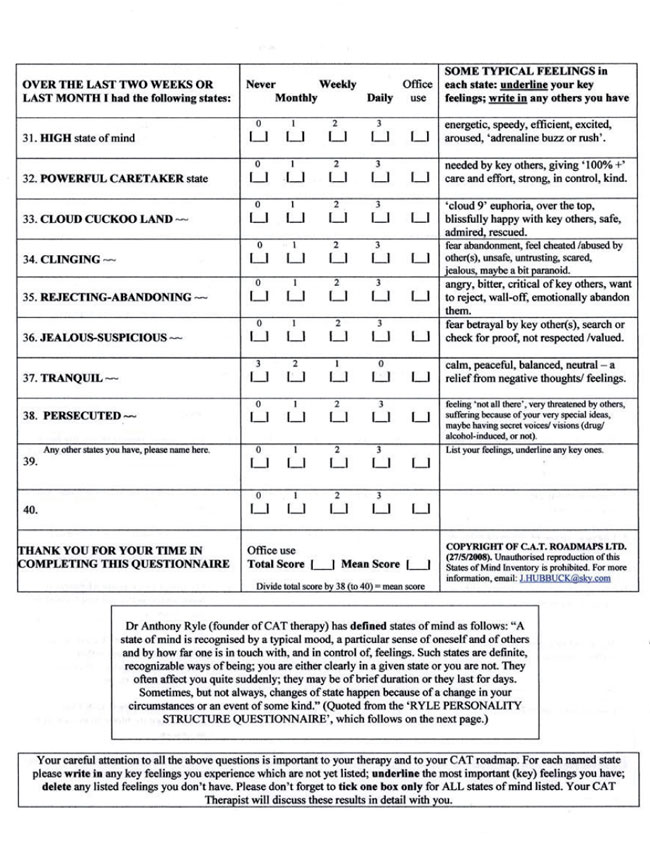
Therefore, in summary, the SCP method, the CAT Psychotherapy File’s 22 named states and the CORE are the foundations of this draft SMI. But I also consulted Lorna Benjamin’s Structural Analysis of Social Behaviour (SASB) simplified cluster model (Benjamin, 1996), Jeffrey Young’s Early Maladaptive Schemas list (Young, 2003); and the so-called ‘Big Five’ personality traits (McCrae and John, 1992). I also reviewed lists of ‘reciprocal roles’ (RRs) in CAT books and articles that have appeared in ‘Reformulation’ journal, from time to time, (including Psaila and Crowley, 2006; and Dunn, 2002). Other writers on states of mind probably need to be consulted before the draft SMI is finalised, such as Horowitz (1979, 1994). But, overall, it is 12 years experience in doing CAT Self-States Sequential Diagram (SSSD) maps, while regularly thinking about variable RR-based states, which led to assessment of the likely 38 most important named states in the draft SMI. The SMI preliminary test results show that patients find it quite manageable to think about 38 questions on mood states, as they do for the 34 questions in the CORE form. So it’s a reasonable assumption that there would be disadvantages in adding yet more states to the SMI list.
Preliminary Test Results
The draft SMI has been tested with 37 patients, initially. The overall results of these tests are presented in Table 1. This table shows there were 10 males and 27 females who filled in the draft SMI. Their ages ranged from 14 to 64. The mean age for males is 42 and 33 for females. 14 patients had clinical scores suggesting BPD. (DSM-IV, American Psychiatric Association, 1994). 23 patients had clinical scores indicating non-BPD. ‘Borderline’ patients recorded experiencing higher numbers of negative states overall (mean 31.9) than non-BPD patients (mean 23.7). This suggests BPD diagnosis and treatment could be aided by integrated SMI and SCP definitions of such higher numbers of poorly controlled, painful states of mind, compared to non-BPD patients. 15 patients were in group therapy and 22 in individual CAT therapy. No patients in this sample reported having difficulties in understanding and filling in this new SMI questionnaire. Very few added their own additional named states, in spaces 39 and 40 on the SMI. Those that did so tended to replicate states already listed in the SMI, but used a different name.
Table 2 contains the rank order of the most frequently named states of mind, by combined daily/ weekly frequency. This rank order will have implications for the list of states included in the SCP questionnaire format. Using the SMI, patients can be helped to identify their most painful and hard to manage states. This information can then be analysed in more detail using the SCP format. This will include the duration, intensity and reciprocal interactions (with key other people) when in these key painful states. The rank order of the top 27 states, for this small sample of BPD patients, is as follows:
Depressed, Can’t Concentrate, Socially Avoidant, Anxious-Confused, Soldiering-On, Frustrated-Bored, Self-Critic, Self-Identity/ Image crisis, Rejecting-Abandoning, Trying Hard to Please, Clinging, Self-Denying, Hurt-Humiliated, Lonely-Isolated, Self-Harming, Zombie-Like, Obsessed-Compelled, Caring-Helpful, Grief-Trauma, Addicted, Rejected-Abandoned, Physically Painful, Powerful Caretaker, Frenetically Active, Hurting-Humiliating, Jealous-Suspicious, Rage.
Of course, an increase in the BPD sample size is likely to change this rank order to some extent. The rank order for the top 27 states, for non-BPD patients, is as follows:
Anxious-Confused, Soldiering-On, Can’t Concentrate, Trying Hard to Please, Caring-Helpful, Depressed, Self-Critic, Socially Avoidant, Frustrated-Bored, OK-Hopeful, Tranquil, Resentful, Self-Identity/ Image crisis, Self-Denying, Hurt-Humiliated, Hurting-Humiliating, Physically Painful, Obsessed-Compelled, Powerful Caretaker, High, Lonely-Isolated, Zombie-Like, Rejected-Abandoned, Panic Attack, Clinging, Grief-Trauma, Addicted.
‘Frenetically Active’, ‘Abused-Victim’ and ‘Critical-Dismissive’ are also ranked as equal 26th with the last two named states above, for non-BPD patients, as shown in Table 2. A quick comparison of these lists shows that the non-BPD patients record having ‘OK-Hopeful’ and ‘Tranquil’ states, that don’t appear in the top 27 states for BPD patients. This would fit with the diagnosis of BPD as also experiencing more marked struggles to control a higher number of negative and painful states of mind. It seems from the above lists that non-BPD patients are more likely to experience ‘High’ and ‘Panic Attack’ states, than BPD patients. The ability to disconnect from panic states is probably related to the major role of dissociation in BPD formation.
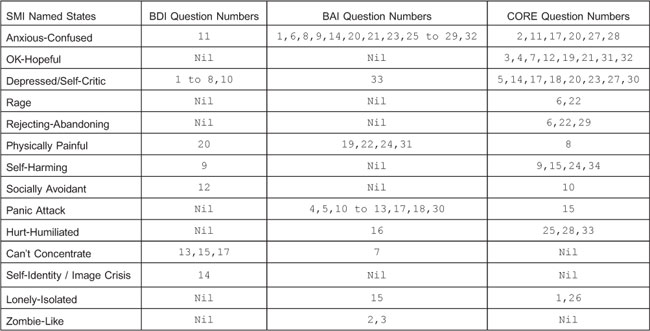
In my individual therapy and CAT group private practice I now give all patients the draft SMI (in Appendix 1), the Ryle Personality Structure Questionnaire (PSQ) (Pollock, et. al., 2001), the Beck Depression Inventory (BDI) (Beck, et. al., 1968), the Burns Anxiety Inventory (BAI) (Burns, 1999), and the CORE (CORE System Group, 2006). Table 3 contains the mean scores for each of these 5 clinical evaluation questionnaires, for the total of 37 patients in this sample, plus the 14 BPD sample. Spearman’s rs rank correlation coefficient tests (Miller, 2006) lead us to accept the prediction (hypothesis Hi): ie. that statistically significant increases in SMI, PSQ, BDI and BAI scores also occur as CORE total scores increase for poor social-psychological functioning. However, the null hypothesis (Ho) is accepted for the PSQ in the BPD sample (n=14) only, as indicated in footnote (1) in Table 3. Table 4 includes the SMI-named states of mind that correspond, approximately, to the individual questions on mood states in the BDI, the BAI and the CORE forms.
The statistically significant correlations between the CORE and the SMI don’t necessarily reflect cause and effect relationships. The SMI, like the CORE, is a general measure of social-psychological functioning. Arguably, the painful states listed in the SMI, and the associated core RRPs, are likely to be the underlying cause of the poor functioning shown in the CORE results. However, the CORE does have documented test validity and reliability, unlike the SMI. Also, the CORE frequency categories have some approximate measures of duration or constancy of mood states, unlike the SMI. But the CORE doesn’t use specific daily, weekly, monthly frequency categories, like the SMI. Nevertheless, some rough equivalent inferences might be made from its frequency categories. The BAI, as its name implies, is a specific measure of anxiety states, not a measure of general social-psychological functioning. Comparisons between the BAI and the SMI show that neither have a duration or constancy measure for mood states. Separate daily, weekly, monthly frequencies are harder to infer from the BAI, than in the CORE. Obviously, the BDI is more a specific measure of depression (as shown in Table 4) and less of a general measure of functioning. Again, it’s hard to infer separate daily, weekly, monthly frequency of mood states from the BDI. Intensity of mood states can be roughly inferred (in varying degrees) from the wording of questions and total scores, in all four questionnaires.
Further Clinical Testing for Validity and Reliability
The ways the PSQ and the CORE have been tested provides some guidance for future testing of the validity and reliability of the SMI. I will need to seek the advice of other CAT colleagues on the best way to proceed with this testing, during 2009. These tests are likely to have implications for further work on integrating the SMI and SCP methods. Ryle (via email 18/11/08) has already given me some welcome guidance.
Ongoing Tests of the SMI in Group Therapy at the Manor Clinic
Dr Philip Milln, Consultant Psychiatrist and Medical Director, has devised a new ‘Day-Care Programme for Depression’ at this Clinic, using CBT and CAT groups. I am providing the CAT groups in this programme and have tested the SMI with 15 group members to date. Since SMI data is integral to the way I practice these groups (Hubbuck, 20/8/08), then these SMI tests are ongoing. After 20 weeks this programme is working well and good therapeutic results are being reported. (Milln, 21/10/08). We plan to ask group members to fill in the above five clinical measures, post-therapy, so as to derive clinical outcome scores. These results could be reported in a later issue of ‘Reformulation’.
Basic Theory Supporting the SMI, Related Core Procedures and SSSDs
Ryle and Kerr (2002) and Ryle (1995) describe the Procedural Sequence Object Relations Model (PSORM) as having universal social-psychological components. Basically, key psychoanalytic and sociological (socialization) theories are restated as painful states of mind being formed and perpetuated, within core RRPs. This formation process starts with: (a) the child’s ‘introjective identification’ of the parental (or caregivers’) attitudes and actions towards the child’s self, often resulting in internalised hurt, neglected, confused, misunderstood, punished, abused, victimised feelings and actions; and (b) the child’s later ‘projective identification’ of the parents and/or caregivers as role models, by externalised angry, hurting, ignoring, neglecting, misunderstanding, punishing, abusing, bullying feelings and actions. From these universal socialization processes children acquire basic reciprocal roles (RRs) which are key parts of early states of mind formation. Ryle notes that such roles and states combine “memory, affect, (attitude) and action organized in relation to the search for, or the experience of, reciprocation.” (Ryle, 1997). Therefore, such states also contain within them the attitudes, or action potentials, of later reciprocal role procedures (RRPs). These arise in later childhood, adolescence and adulthood, as habitual, repetitive, often core stereotypical sequences of mutual interaction with significant others in pursuit of key life goals. While Ryle cautions that RRPs need to be regarded as a ‘heuristic device’, he also points out that:
“All such procedures, once established, will be stable due to the fact that the confirming reciprocations of the enacted role can usually be elicited from others, leaving the core repertoire unchanged……..the PSORM offers, in this way, a more general understanding of the stability of personality.” (Ryle, 1995). And again he states: “It should be emphasised that ‘role’, as used here, implies action linked to memory, meaning, affect and expectation. The subjective experience of playing a role can be described as a state of mind or state of being, terms which must be distinguished from reciprocal role procedure, which is essentially a theoretical construct.” (Ryle and Kerr, 2002).
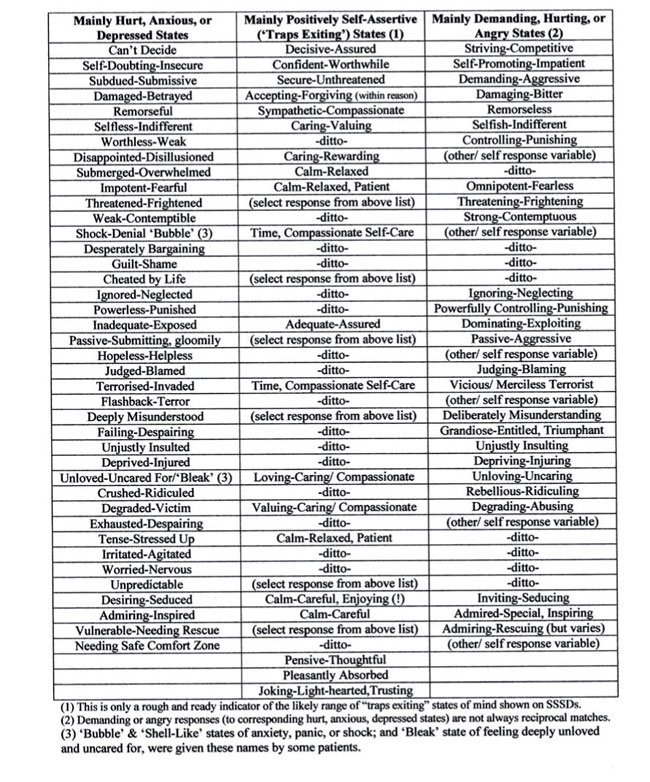
The evidence from my own individual and group CAT practice is that patients do have an obvious tendency to recognise the general, often stereotypical states of mind named in the draft SMI and the SCP. The use of the CAT Psychotherapy File also shows that there is an equivalent, near-universal tendency to recognise the following social-psychological ‘traps’: Depressed Thinking, Fear of Hurting Others, Avoidance, Trying to Please, Social Isolation and Low Self-Esteem. Patients nearly always recognise such general (PSORM and RRP-based) traps processes, within themselves. However, as implied above, these six traps are basically ‘heuristic devices’ that are not immutable.
In my recent way of practising CAT I conflate the six above-named traps into just two basic traps. The wording of all these traps states, basically: (1) we start off by feeling either depressed (worthless), or anxious (fearful, ineffective, uncertain, under-confident); (2) we then feel that we have handled things badly, that others ignore or abuse us, take advantage of us; (3) so we avoid situations, don’t stand up for our rights, hang back, hide away, give up trying to do things; (4) then we end up feeling more depressed, or more anxious. It’s evident from this that these six traps do conflate into a universal “Depressed (and Anxious) Thinking/ Social Avoidance Trap” tendency. The SMI also has named “Socially Avoidant” and “Depressed” states. Because of this conflation, perhaps in reality, then it’s not surprising that BPD patients often identify all these traps. So it’s also not unreasonable to regard the ‘Low Self-Esteem Trap’ as a function of depressed thinking. The wording of this particular trap in the File starts and ends with feeling “worthless”, which is a key descriptor (adjective) of depression. This conflation then makes the SSSD mapping process easier in practise. Dilemmas and snags can also be conflated. Therefore, consideration needs to be given to possible replacement of the Psychotherapy File, after further integration of the SMI and SCP methods.
It’s less clear from the CAT File’s wording of the ‘Trying to Please Trap’ and the ‘Fear of Hurting Others Trap’ that there is also something more fundamental going on in these two traps. As CAT practitioners know, contained within the PSORM, are the basic attachment, love and care needs of the human infant. Lavinia Gomez’s chapter on ‘John Bowlby and Attachment Theory’ summarises the deep importance to the child’s sense of security that these needs are adequately met. As a rough guess, maybe children need parents (or caregivers) to provide a 60-70% level of attunement and effort in meeting these basic emotional care needs. If they are not adequately met, then the seeds of anxiety, depression and personality disorder are possibly sown for adult life. (Gomez, 1997). And the seeds are probably sown for most of the key RR-based states named in the SMI, as adults. Also, the seeds are sown for the powerful, perhaps unending search in adult life, for ‘perfect attachment, love and ideal care’. This search is often shown on SSSDs as “A Trying Hard to Please/ Ideal Care Trap”. These maps then commonly contain the words ‘Ideal Care/ Perfect (100%) Standards’ (of effort and performance in key life roles and goals, such as family, work and love life). This trap also sometimes contains the words: “I fear hurting others, because they could hurt me back.” While I don’t want to map out a typical Ideal Care Trap here, such maps do commonly contain the following states from the SMI: “Soldiering-On”, sometimes “Zombie-Like”, “Trying Hard to Please”, sometimes “Obsessed-Compelled” and “High”, sometimes in “Powerful Caretaker” and “Cloud Cuckoo Land” states, (occasionally in a “Perfect Care Bubble”), sometimes ending up in “Clinging”, “Jealous-Suspicious”, “Rejected-Abandoned”, or “Rejecting-Abandoning” states of mind.
Incidentally, I often say to my individual and group patients that Steven Spielberg’s film ‘AI: Artificial Intelligence’ is a memorable futuristic fairy tale, which captures, metaphorically, the human child’s universal search for perfect attachment, or ideal love and care. This can often end up like a desperate odyssey, in adult life. And I often say to patients that we tend to be powerfully conditioned, by social, economic, technological, and political processes towards perfect attachment to products, services and lifestyle, not just to key individuals. ‘Perfect Competition’ economic theory has been a powerful underlying force in the organisation of modern, market-driven societies, like the US and the UK. (Lipsey and Chrystal, 2007). And it’s probably got us into the current economic recession, but hopefully not another “Great Depression.” Mark Dunn (in supervision, 24/11/08) suggested a ‘Jack and the Beanstalk’ metaphor, where bankers and hedge fund managers have “sold the cow for the magic beans.”
Other States of Mind Not Included
Appendix 2 contains a long list of common states of mind that are not included in the draft SMI. Some of these were self-identified by patients in their SDP forms, as additional named states. But most of these extra states have been derived from my own social and clinical observations and from CAT colleagues work in identifying RR-based states. However, these were judged as less important for the draft SMI, for the following reasons: (a) many are already subsumed in other named states in the SMI; (b) some are often named in typical SSSDs that I collaborate on with individual and group patients. In listing all these states (about 80) this probably does go some way to answering the question: “Does every waking minute of a person’s conscious life have an underlying, nameable state of mind?” Obviously I can’t prove this, but my gut feeling (supported by the PSORM) is that the likely answer is “yes”.
Conclusions
My previous article indicated the high therapeutic value the SCP method can deliver to patients. The SMI and the related core RRP/ SSSD mapping process in groups also seems to give high therapeutic value. In filling in the SMI (and the SCP), many patients have said to me that they had never really thought like this before about their very painful states of mind, or their related procedural sequences (traps). And their individual SSSD is often a welcome revelation to them, providing them with the hope of being able to ‘positively exit’ their negative states and traps. Being able to turn quickly to the SMI, in individual and group sessions, gives the unmistakeable (reciprocal) feeling of having a good therapeutic tool readily available. Moreover, the regular exchange of SMI information between CAT group members tends to confirm for them the generality or commonality of such named states of mind and related traps. Perhaps the real bonus of this group mapping method, is that it delivers good enough CAT maps more quickly, more economically, to more patients in serious need, than in 1:1 therapies.
In his recent article Ryle (2007a) wrote that treating BPD patients without the benefit (in effect) of a good SSSD “can resemble a boxing match taking place in the dark.” The evidence from the draft SMI presented here is likely to enhance the possibility of valid and reliable SSSDs. The SMI has already helped to show that each BPD patient probably has his/ her own “internal boxing match in the dark”, (beating self up in “Self-Critic” and “Self-Identity/ Image” crisis states) as his/ her own mind (or brain) struggles to cope with at least 8 more (or about 35% more) named painful states on average, than for non-BPD patients. This needs further investigation, given the central importance of states of mind (within core RRPs) to brain functioning and personality development. This may have significant implications for future psychiatric and psychotherapy research. In my further research plans, I expect to give due weight to Anthony Giddens’ (ex-Director, London School of Economics) sociological theories of self- and social reflexivity, gender-based emotional democracy, family and social group conflict resolution. (Giddens, 2003; 2006). Ryle (via email, 14/11/08) has encouraged this broader focus for CAT.
I am grateful to Dr Ryle for taking time to collaborate with me on states of mind research. Also, I’m grateful to Dr Milln for the support he has given to this CAT group therapy work. Hopefully, further research will lead to full integration of the SCP and SMI methods. [Any comments please to: J.Hubbuck@sky.com].
References
Beck, A. T., Ward, C. H., Mendelson, M., Mock, J. E., and Erbaugh, J. K., (1968). An Inventory for Measuring Depression. Archives of General Psychiatry, 4, 561-571.
Burns, D. (1999). The Feeling Good Handbook: Revised Edition. Plume (Penguin Books). 43-44.
Benjamin, L. S. (1996). Interpersonal Diagnosis and Treatment of Personality Disorders: Second Edition. New York, The Guilford Press.
Clinical Outcomes in Routine Evaluation: CORE System User Manual (2006). Mental Health Foundation and CORE System Group.
Diagnostic and Statistical Manual of Mental Disorders: Fourth Edition DSM-1V (1994). 301.83 Borderline Personality Disorder, American Psychiatric Association. Washington, DC. 650-654.
Dunn, M. (2002). To boldly go….(a view of CAT after 15 years), ACAT News, 16, 5-6.
Giddens, A. (2003). Modernity and Self-Identity: Self and Society in the Late Modern Age. Cambridge, Polity Press.
Giddens, A. (2006). Sociology: 5th Edition. Cambridge, Polity Press.
Goleman, D. (2004). Emotional Intelligence and Working with Emotional Intelligence. Bloomsbury Publishing.
Gomez, L. (1997). An Introduction to Object Relations. London, Free Association Books.
Horowitz, M. J. (1979). States of Mind. New York, Plenum Press.
Horowitz, M. J., Milbrath, C., Ewart, M., Sonnebon, D. and Stinson, R. (1994). Cyclical patterns in states of mind in psychotherapy. American Journal of Psychiatry, 151, 1767-1770.
Hubbuck, J. (2008). The States Description Procedure: Some Clinical Implications for the Self-States Sequential Diagram (SSSD), Reformulation: Theory and Practice in CAT, 30, 46-53.
Hubbuck, J. (20/8/08). Manor Clinic CAT Groups for Depression and Anxiety: A Summary of the Purpose and Method of Drawing Up Individual CAT Roadmaps in a Group Therapy Setting. (Available on request to: J.Hubbuck@ sky.com).
Lipsey, R. and Chrystal, A. (2007). Economics: Eleventh Edition. Oxford University Press, 136-159.
McCrae, R. R. and John, O. P. (1992). An introduction to the five-factor model and its applications. Journal of Personality, 60, 175-215.
Miller, S. (2006). Experimental Design and Statistics: Second Edition. Routledge
Milln, P. T. S. (21/10/08). Meeting to discuss progress on CBT and CAT group therapy at the Manor Clinic, Southampton. Patients report a high level of satisfaction.
Pollock, P., Broadbent, M., Clarke, S., Dorrian. A. J., and Ryle, A. (2001). The Personality Structure Questionnaire (PSQ): A measure of the multiple self-states model of identity disturbance in Cognitive Analytic Therapy, Clinical Psychology and Psychotherapy, 8, 59-72.
Psaila, C. L. and Crowley, V. (2006). Cognitive Analytic Therapy in People with Learning Disabilities: An Investigation into the Common Reciprocal Roles found within this Client Group, Reformulation: Theory and Practice in CAT, 27, 5-11.
Ryle, A. (2007a). Investigating the Phenomenology of Borderline Personality Disorder with the States Description Procedure: Clinical Implications. Clinical Psychology and Psychotherapy, 14, 5, 329-341.
Ryle, A. (2007b). States Characterisation Procedure (SCP): For supporting the reformulation of patients with borderline/ dissociative features. Reformulation: Theory and Practice in CAT, 29, 9-11.
Ryle, A. (1997). Cognitive Analytic Therapy and Borderline Personality Disorder: The Model and the Method. John Wiley & Sons, 27.
Ryle, A., ed. (1995). Cognitive Analytic Therapy: Developments in Theory and Practice. John Wiley & Sons.
Ryle, A. and Kerr, I. B. (2002). Introducing Cognitive Analytic Therapy: Principles and Practice. John Wiley & Sons.
Ryle, A. and Golynkina, K. (2000). Effectiveness of time-limited Cognitive Analytic Therapy for borderline personality disorder: factors associated with outcome. British Journal of Medical Psychology, 73, 197-210.
Siegel, D. J. (1999). The Developing Mind: How Relationships and the Brain Interact to Shape Who We Are. New York, The Guilford Press.
Young, J. E., Klosko, J. S., and Weishaar, M. E. (2003). Schema Therapy: A Practitioners Guide. New York, The Guilford Press.
Table 1
Total Sample of Patients Completing the Draft States of Mind Inventory (SMI) (n=37); by Sex, Mean Age, Number with Borderline Personality Disorder (BPD) Clinical Scores and Non-BPD Clinical Scores, Mean Number of SMI States Identified by BPD and Non-BPD Patients; and Number of Patients in Group or 1:1 CAT Therapy
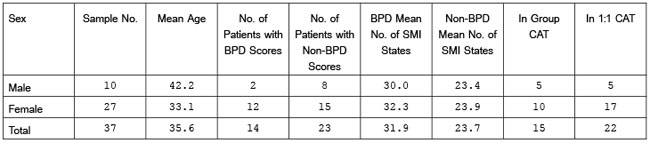
BPD and non-BPD clinical evaluation scores are derived from the Ryle Personality Structure Questionnaire (PSQ), (Pollock, et. al. 2001); the Beck Depression Inventory (BDI), (Beck, et. al. 1968); the Burns Anxiety Inventory (BAI), (Burns, 1999); and the Clinical Outcomes in Routine Evaluation questionnaire (CORE), (Core System User Manual, 2006). Ryle’s Severity Index was not applied in this study, due to time constraints. (Ryle and Golynkina, 2000).
Table 2
Number and Percentage of Patients Experiencing the Draft SMI 38 Named States of Mind, plus Rank Order of these States, by Combined Daily/ Weekly Frequency, for the Total Sample (n=37), BPD Sample (n=14) and Non-BPD Sample (n=23)
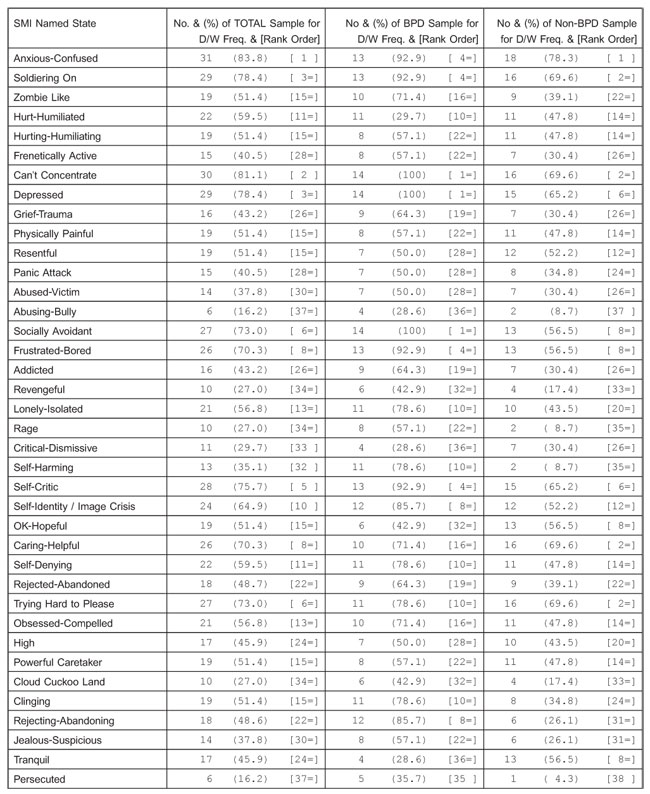
Table 3
Mean Total Scores for the Draft SMI, the PSQ, BDI, BAI and CORE Clinical Evaluation Questionnaires for this Total Sample (n=37), by Sex, Mean BPD (n=14), Mean Non-BPD (n=23); and Spearman’s (1) Rank Correlation Coefficients for Statistical Significance
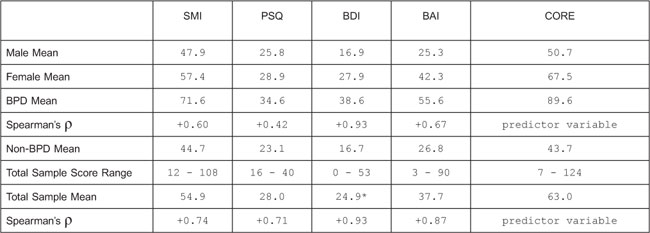
*Estimated BDI score for one female non-BPD patient only.
(1) Spearman’s ρ (one-tailed test) for non-parametric data was applied to the SMI, PSQ, BDI, BAI total scores, for the BPD sample (N=14) and for the total sample (N=37). The CORE was assumed to be the predictor (independent) variable. The hypothesis (Hi) is referred to in the text and is accepted. Significant correlations do not necessarily reflect cause and effect relationships between variables. rs values shown in the above table are all significant at P .025 level, with the exception of the PSQ for the BPD sample. In this case the null hypothesis (Ho) is accepted: ie. that there is no relationship between the increase in PSQ and CORE total scores for the BPD sample only. The BDI (+0.93) is the nearest to +1 (perfect positive correlation) with the CORE.
Table 4
Named States of Mind in the Draft SMI broadly corresponding to the Question Numbers
in the BDI, BAI and CORE Clinical Evaluation Questionnaires
Appendix 1. SMI
Appendix 1. SMI cont.
Appendix 1. SMI cont.
Appendix 2. Some Named States Not Included In The Draft SMI
Many of these states are subsumed in various named SMI states, or regularly named and subsumed in CAT maps (SSSDs) that I collaborate on with patients.

Full Reference
Hubbuck, J., 2008. Draft States of Mind Inventory. Reformulation, Winter, pp.15-25.Search the Bibliography
Type in your search terms. If you want to search for results that match ALL of your keywords you can list them with commas between them; e.g., "borderline,adolescent", which will bring back results that have BOTH keywords mentioned in the title or author data.
Related Articles
The States Description Procedure
Hubbuck, J., 2008. The States Description Procedure. Reformulation, Summer, pp.46-53.
The PSQ Italian Standardisation
Fiorani, C. and Poggioli, M., 2011. The PSQ Italian Standardisation. Reformulation, Winter, pp.49-52.
States Characterisation Procedure (SCP) for supporting the reformulation of patients with borderline/dissociative features
Ryle, A., 2007. States Characterisation Procedure (SCP) for supporting the reformulation of patients with borderline/dissociative features. Reformulation, Winter, pp.9-11.
The States Description Procedure
Ryle, T., 2003. The States Description Procedure. Reformulation, Autumn, pp.13-16.
Letters to the Editors: Improve Your Reformulation and Contribute to Research - Try the States Description Procedure (SDP)
Ryle, T., 2003. Letters to the Editors: Improve Your Reformulation and Contribute to Research - Try the States Description Procedure (SDP). Reformulation, Spring, p.5.
Other Articles in the Same Issue
“My Life in Pictures†OCD and CAT
Kimber-Rogal, N., 2008. “My Life in Pictures†OCD and CAT. Reformulation, Winter, pp.7-13.
CAT and the Media
McCormick, L., 2008. CAT and the Media. Reformulation, Winter, p.6.
Draft States of Mind Inventory
Hubbuck, J., 2008. Draft States of Mind Inventory. Reformulation, Winter, pp.15-25.
Letter from the Editors
Elia, I., Jenaway, A., 2008. Letter from the Editors. Reformulation, Winter, p.3.
Looking at a Therapeutic Relationship In CAT
Raymond, C., 2008. Looking at a Therapeutic Relationship In CAT. Reformulation, Winter, pp.26-27.
Measuring Outcomes in CAT
Freeman, E., Williams, L., 2008. Measuring Outcomes in CAT. Reformulation, Winter, p.14.
Relationships and CAT
Kimber-Rogal, N., 2008. Relationships and CAT. Reformulation, Winter, pp.28-29.
Statutory Regulation Update
Westacott, M., 2008. Statutory Regulation Update. Reformulation, Winter, pp.3-4.
The CAT Articles Review
Knight, A., 2008. The CAT Articles Review. Reformulation, Winter, p.30.
Help
This site has recently been updated to be Mobile Friendly. We are working through the pages to check everything is working properly. If you spot a problem please email support@acat.me.uk and we'll look into it. Thank you.
